Mykhaylo Solomonyuk
Private practice
Vilnius, 09302, Lithuania, Giedraiciu g.41-103
Cell Phone +37065385476. E- mail address. solomonyuk@gmail.com
In the article were used 1 tables and 6 illustrations.
In the 1997 graduated from Ukrainian Medical Stomatological Academy (the city of Poltava). 2000-2002 Clinical Residency at the Chair of stomatology of the National Medical Academy of Post-Graduate Education named after P.L.Shupic. 2002-2006 Full-time postgraduate courses at the National Medical Academy of Post-Graduate Education named after P.L.Shupic. 2007-2008 Completed full training course for foreign doctors on the department of orthodontics of National University of Daegu (South Korea). Membership of the American Association Orthodontists (AAO).
Summary
Кey words: microimplants, coil spring, Class II .
In this article we consider the clinical case of treatment of the patient with Class II Engle using microimplants for distalisation of upper molar. Application of microimplants has allowed to spend treatment without removal of a teeth, to improve aesthetic parametres of the person at the patient, to establish class І Engle. The Effective control distal movement of a teeth using microimplants allows to reduce terms of orthodontic treatment.
Class II Correction with Microscrews Implants
Historically, views on orthodontic treatment with or without the extraction of certain teeth have changed multiple times [1].
During Edward Angle’s era, orthodontic treatment was primarily conducted without extractions. However, the lack of stable support in orthodontic treatment often negatively impacted the facial profile [2].
Charles Tweed proposed a new treatment technique based on the principles of anchorage through the distal inclination of posterior teeth. Using cephalometric analysis, he justified the necessity of premolar extractions based on the diagnostic triangle [3].
Currently, the necessity of preserving teeth, especially first premolars, in orthodontic treatment is actively discussed. Several researchers have introduced the concept of functional occlusion, based on the principles of gnathology. They consider the extraction of premolars in orthodontic treatment unacceptable, as it leads to an imbalance in the functioning of the masticatory system and can trigger the development of TMJ dysfunction [4].
Among non-extraction methods of treating orthodontic anomalies, the most common is distalization [5].
One of the first appliances used for distalization was the Headgear. However, wearing the Headgear as a treatment method is rejected by many patients due to aesthetic and social considerations, and it requires full commitment to wearing the appliance for at least 18 hours a day [6]. Among most intraoral appliances for distalization, the most common is the Pendulum and its modifications. However, the need for laboratory stages to fabricate the appliance and the duration of treatment stages have led to the creation of other systems [7].
We propose a method for moving the upper dental arch using microimplants and sliding mechanics.
A 21-year-old female patient visited the clinic with complaints of an unattractive smile and dental crowding (Fig. 1). External examination showed a symmetrical, proportionate face with a mesocephalic type. The profile was convex, lips were apart at rest, and breathing was mixed. The chin and nasolabial folds were moderately pronounced.
Intraoral examination revealed a Class II molar relationship according to Angle, complicated by deep incisal occlusion. Model analysis showed crowding in the upper dental arch of 7 mm and in the lower arch of 5 mm.
The Panoramic did not reveal any resorption or inflammatory phenomena. The root canals of tooth 46 are filled, and the lower third molars 18, 28, and 48 are retained.
Decoding of the lateral cephalogram before treatment revealed a skeletal Class I – ANB angle of 4º, SNA angle of 79º, SNB angle of 75º, and mandibular angle FMA (the angle between the Frankfurt plane and the mandibular plane) of 27º (Table 1). The position of the upper incisors U1 to FH (the angle formed by the axis of the upper central incisors U1 to the Frankfurt horizontal FH) is 109º. The relation of the lower central incisors – IMPA (the angle between the axis of the lower central incisors and the mandibular plane) is 105º. The inclination angle of the occlusal plane to the Frankfurt horizontal is below the average values (FH to Occ P 18º). The symmetrical position of the anterior facial height in relation to the posterior – the PFH/AFH index is 0.7 (Fig. 2).
Based on the data from clinical examinations, anthropometric study of jaw models, and the use of additional special methods of investigation such as lateral cephalogram and Panoramic, the diagnosis was established: permanent dentition, Angle Class II, complicated by deep incisal occlusion, crowding of the teeth in the anterior segment of the upper and lower dental arches of the second degree, skeletal Class I.

Fig. 1. Photographs of the patient before treatment
The treatment stages necessary for the correction of the identified pathology consisted of the following:
- Sanitation of the oral cavity.
- Elimination of crowding in the upper and lower dental arches.
- Normalization of the sagittal and vertical relationships of the upper and lower central incisors.
- Correction of deep incisal occlusion.
- Improvement of the facial profile.
- Establishing canine and molar relationships to Angle Class I, achieving functional occlusion. To address these objectives, several treatment options were proposed to the patient. The first option involved the extraction of premolars in the upper and lower dental arches. The patient categorically refused premolar extractions. The second alternative treatment plan was the movement of the upper teeth using microimplants for support and the extraction of the retained lower wisdom teeth.
The patient agreed to this treatment plan.
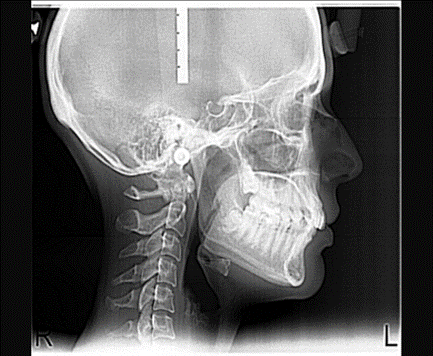
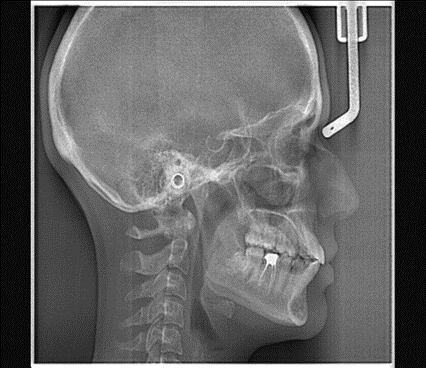
Fig. 2. Pre and Posttreatment lateral cephalometric radiographs
Table 1.Cephalometric measurements
| Measurements Pretreatment Posttreatment Retention |
| SNA 82 79 79 SNB 80 75 77 ANB 2 4 2 FMA 25 27 23 PFH/AFH 0,8 0,7 0,8 FH к Occ P 10 18 12 Ui к FH 114 109 118 IMPA 90 105 105 Z-angle 75 75 80 |
Fixed appliances “Roth prescription” with a slot of 0.022 inches and an initial nickel-titanium (Ni-Ti) archwire of 0.014 inches, followed by 0.016 and 0.016 × 0.025 inches, were installed. After aligning the dental arches, a stainless steel archwire of 0.019 × 0.025 inches was placed on the brackets of the upper and lower dental arches. To create absolute anchorage, 2 microimplants (diameter, 1.5 mm; length, 8 mm from “Dentos AbsoAnchor,” Korea) were placed in the inter-root space between the second premolars and first molars in the upper jaw at a diagonal angle of 60° to the bone surface. Hooks were soldered onto the upper stainless steel archwire between the lateral and central incisors. For the movement of the upper teeth, closed nickel-titanium springs were installed from the head of the microimplant to the soldered hooks on the archwire, each with a force of 250 mg (Fig. 3).

Fig. 3. 2 microimplants placed in the upper jaw
The closed coil springs were removed after achieving a Class I molar relationship according to Angle. To prevent the wedging effect of the teeth due to the distal movement of the molars, an increase in the FMA angle, rotation of the occlusal plane, and open bite, the posterior teeth were intruded using an elastic chain with a force of 150 g, attaching it from the heads of the micro screws around the archwire in the area of the second premolars and first molars.
Treatment Results
The fixed appliances were removed 15 months after the start of treatment. Analysis of facial photographs revealed a noticeable improvement in the facial profile. Intraoral photographs showed that the dental arches were aligned (Fig. 4). Model analysis demonstrated average values for the sagittal and vertical relationships of the incisors. The dental arches had an Angle Class I relationship, with the midline coinciding in the upper and lower dental arches. Diagnosis in the articulator in the resting state revealed tight inter-cusp contact between the dental arches, absence of premature contacts during lateral movements of the mandible, a frontal guidance, and canine guidance on both sides.

Fig. 4. Photographs of the patient after treatment
Cephalometric analysis showed a decrease in the FMA angle and the FH to Occ P angle. There was an increase in SNB and Z-angle. The PFH/AFH index was 0.8. In the Panoramic, the tooth roots were parallel, and there was no resorption (Fig. 5). The microimplants provided complete anchorage during distalization, with no signs of mobility or loss observed during the treatment process.
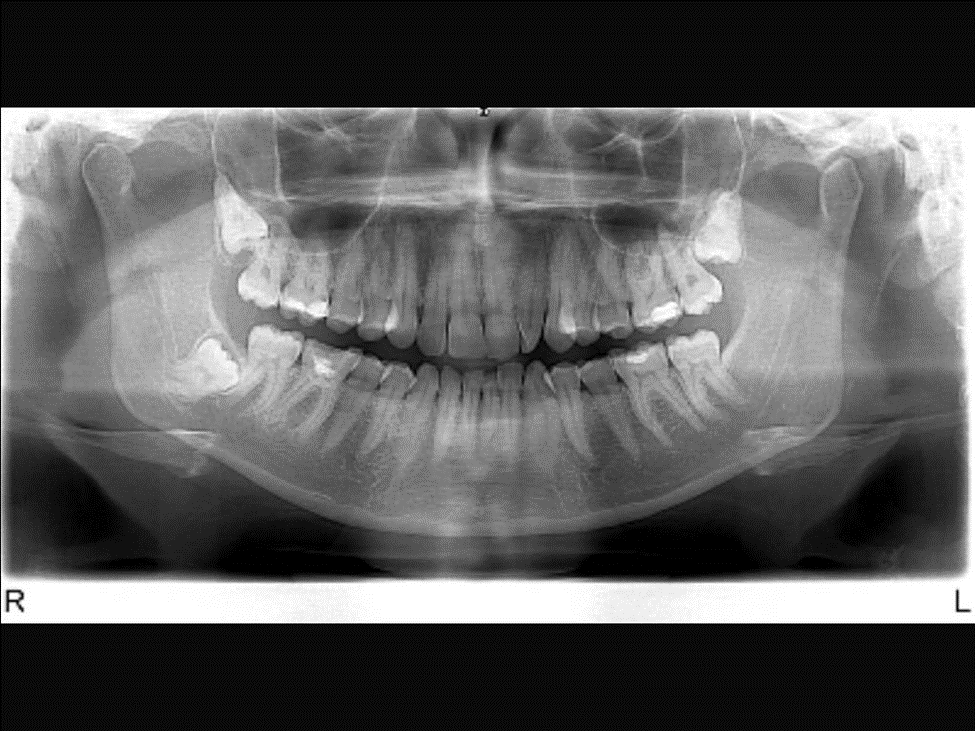
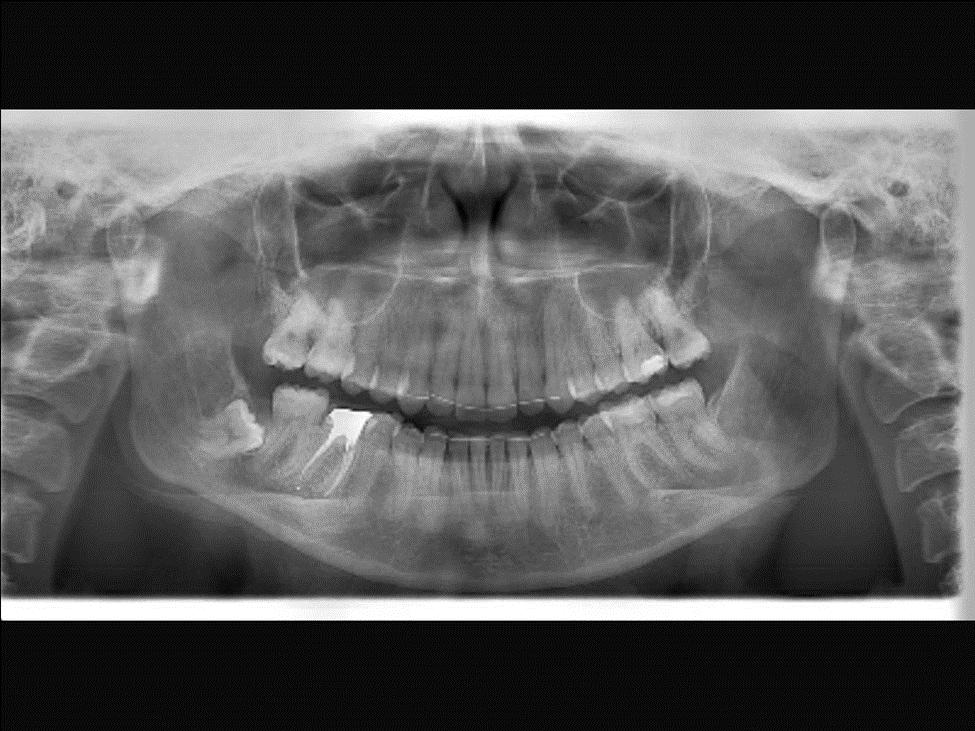
Fig. 5. Pre and Posttreatment panoramic radiographs
After 1 year retention, clinical examination showed no relapse and stability of the previously achieved results. The canine and molar relationships were Angle Class I. There was no crowding of the teeth in the anterior segment of the upper and lower dental arches. The dental arches had a proper shape, with normal sagittal overjet and vertical occlusion. There were no symptoms from the temporomandibular joint (Fig. 6).

Fig. 6. Photographs of the patient after 1 year Retention
Analysis and Discussion
The movement of upper lateral teeth using microimplants with sliding mechanics provides maximum mechanical advantages compared to traditional methods. There is no need for preliminary use of a distalizing appliance – treatment begins directly with the installation of a fixed system.
The key success factor in orthodontic treatment is the choice of anchorage or support. In this clinical case, microimplants were used for stable anchorage. Their application is highly preferable due to ease of placement, minimal anatomical restrictions during insertion, absence of waiting time for osseointegration, and the possibility of immediate loading after placement. Proper selection of length, diameter, and precise placement is crucial for their stable anchorage in bone tissue throughout the treatment period. The choice of microimplant diameter depends on the width of the inter-radicular space, determined by periapical contact radiographs or fragments of computed tomography scans. When adequate space is available, it is recommended to install microimplants with a diameter of at least 1.5 mm in the upper and lower jaws. In cases where space is limited due to proximity of roots, microimplants with a minimum diameter of 1.2-1.3 mm are screwed in.
Length does not have a decisive role because the main fixation occurs between the microimplant and cortical bone. However, on the upper jaw, it should be installed no less than 6 mm, and on the lower jaw – 5 mm. It is best to insert the microimplant at an oblique angle of 30-60º to the bone surface. This direction reduces the risk of root damage during placement. It encompasses a larger volume of cortical bone, increasing the anchoring strength. Microimplants are preferably placed 6-8 mm from the gingival margin. This provides good access to the microscrew head for using various types of elastic traction.
Conclusions
- Using microimplant anchorage allows for molar movement without losing anchorage in both horizontal and vertical planes.
- The most stable effect is observed in patients with a low FMA.
- Crowding of the dental arch greater than 7 mm, high IMPA, and high FMA may indicate the need for extraction of individual teeth.
- For stable anchorage in the upper jaw, microimplants should be installed with a length of no less than 8 mm.
- The success of microimplant placement depends on the patient’s bone density, the orthodontist’s clinical skills, differential diagnostic stages conducted, site and direction chosen for microimplant placement, and oral cavity hygiene.
References
- Proffit W.R. Contemporary Orthodontics. // 2nd ed. St Louis, Mo: CV Mosby. – 1993. – P. 306 – 307.
- Angle EH. The treatment of malocclusion of the teeth, 7th Edition, Philadelphia SS white, 1907:64.
- Tweed CH. A philosophy of orthodontic treatment // Am. J. Orthod. Oral. Surg. 1945. –№31. –P.74–103.
- Cetlin N.M., Ten Hoeve A. Non extraction treatment // J.Clin.Orthod. – 1993. – Vol. 17. – P. 396 – 413.
- Gianelly A.A.,Vaitas A.S., Thomas W.M. The use of magnets to move molars distally // Am. J. Orthod. Dentofac. Orthop. – 1998. – Vol. 96. – P.161 – 167.
- Muse D.S., Fillman M.J., Emmerson W.F., Mitchell R.D. Molar and incisor changes with Wilson rapid molar distalisation // Am. J. Orthod. Dentofac. Orthop. – 1993. – Vol. 104. – P.556-565.
- Hilgers J.J., The pendulum appliance for Class II non-compliace therapy // J. Clin. Orthod. – 1992. – Vol. 26. – P. 706 – 714.



0 Comments